Psoriasis
Contents:
When to Contact a Medical Professional
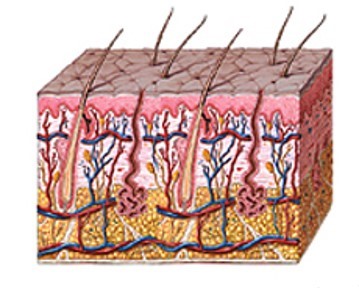
Psoriasis is a common skin condition that causes skin redness and irritation. Most people with psoriasis have thick, red skin with flaky, silver-white patches called scales.
Causes
Psoriasis is very common. Anyone can get it, but it most often begins between ages 15 and 35.
You cannot catch psoriasis or spread it to others.
Psoriasis seems to be passed down through families. Doctors think it may be an autoimmune condition. This occurs when the immune system mistakenly attacks and inflames or destroys healthy body tissue.
Normal skin cells grow deep in the skin and rise to the surface about once a month. When you have psoriasis, this process takes place too fast. Dead skin cells build up on the skin's surface.
The following may trigger an attack of psoriasis or make the condition harder to treat:
- Bacteria or viral infections, including strep throat and upper respiratory infections
- Dry air or dry skin
- Injury to the skin, including cuts, burns, and insect bites
- Some medicines, including antimalaria drugs, beta-blockers, and lithium
- Stress
- Too little sunlight
- Too much sunlight (sunburn)
- Too much alcohol
Psoriasis may be worse in people who have a weak immune system. This may be due to:
- AIDS
- Autoimmune disorders (such as rheumatoid arthritis)
- Cancer chemotherapy
Some people with psoriasis may also have arthritis (psoriatic arthritis).
Symptoms
Psoriasis can appear suddenly or slowly. Many times, it goes away and then comes back.
The main symptom of the condition is irritated, red, flaky patches of skin. Patches are most often seen on the elbows, knees, and middle of the body. But they can appear anywhere, including on the scalp.
The skin may be:
- Itchy
- Dry and covered with silver, flaky skin (scales)
- Pink-red in color (like the color of salmon)
- Raised and thick
Other symptoms may include:
- Genital sores in males
- Joint pain or aching
- Nail changes, including thick nails, yellow-brown nails, dents in the nail, and a lifting of the nail from the skin underneath
- Severe dandruff on the scalp
There are five main types of psoriasis:
- Erythrodermic -- The skin redness is very intense and covers a large area.
- Guttate -- Small, pink-red spots appear on the skin.
- Inverse -- Skin redness and irritation occurs in the armpits, groin, and in between overlapping skin.
- Plaque -- Thick, red patches of skin are covered by flaky, silver-white scales. This is the most common type of psoriasis.
- Pustular -- White blisters are surrounded by red, irritated skin.
Exams and Tests
Your doctor or nurse can very often diagnose this condition by looking at your skin.
Sometimes, a skin biopsy is done to rule out other possible conditions. If you have joint pain, your doctor may order x-rays.
Treatment
The goal of treatment is to control your symptoms and prevent infection.
Three treatment options are available:
- Skin lotions, ointments, creams, and shampoos. These are called topical treatments.
- Pills or injections that affect the body's immune response, not just the skin. These are called systemic, or body-wide, treatments.
- Phototherapy, which uses light to treat psoriasis.
TREATMENTS USED ON THE SKIN (TOPICAL)
Most of the time, psoriasis is treated with medicines that are placed directly on the skin or scalp. These may include:
- Cortisone creams and ointments
- Creams or ointments that contain coal tar or anthralin
- Creams to remove the scaling (usually salicylic acid or lactic acid)
- Dandruff shampoos (over-the-counter or prescription)
- Moisturizers
- Prescription medicines containing vitamin D or vitamin A (retinoids)
SYSTEMIC (BODY-WIDE) TREATMENTS
If you have very severe psoriasis, your doctor will likely recommend medicines that suppress the immune system's faulty response. These medicines include methotrexate or cyclosporine. Retinoids such as acitretin can also be used.
Newer drugs called biologics are used when other treatments do not work. Biologics approved for the treatment of psoriasis include:
- Adalimumab (Humira)
- Etanercept (Enbrel)
- Infliximab (Remicade)
- Stelara
PHOTOTHERAPY
Some people may choose to have phototherapy.
- Phototherapy is a medical treatment in which your skin is carefully exposed to ultraviolet light.
- Phototherapy may be given alone or after you take a drug that makes the skin sensitive to light.
- Phototherapy for psoriasis can be given as ultraviolet A (UVA) or ultraviolet B (UVB) light.
OTHER TREATMENTS
If you have an infection, your doctor will prescribe antibiotics.
AT HOME CARE
Follow these tips at home:
- Taking a daily bath or shower can help your psoriasis. Try not to scrub too hard because this can irritate the skin and trigger an attack.
- Oatmeal baths may be soothing and may help to loosen scales. You can use over-the-counter oatmeal bath products. Or, you can mix 1 cup of oatmeal into a tub of warm water.
- Keeping your skin clean and moist and avoiding your specific psoriasis triggers may help reduce the number of flare-ups.
- Sunlight may help your symptoms go away. Be careful not to get sunburned.
- Relaxation and antistress techniques may be helpful. The link between stress and flares of psoriasis is not well understood, however.
- Limiting the alcoholic beverages you drink may help keep psoriasis from getting worse.
Support Groups
Some people may benefit from a psoriasis support group.
Outlook (Prognosis)
Psoriasis is a life-long condition that can be controlled with treatment. It may go away for a long time and then return. With proper treatment it will not affect your overall health. Some people with psoriasis have a type of arthritis.
When to Contact a Medical Professional
Call your health care provider if you have symptoms of psoriasis or if the skin irritation continues despite treatment.
Tell your doctor if you have joint pain or fever with your psoriasis attacks.
If you have symptoms of arthritis, talk to your dermatologist or rheumatologist.
Go to the emergency room or call the local emergency number (such as 911) if you have a severe outbreak that covers all or most of your body.
Prevention
There is no known way to prevent psoriasis. Keeping the skin clean and moist and avoiding your specific psoriasis triggers may help reduce the number of flare-ups.
Doctors recommend daily baths or showers for persons with psoriasis. Avoid scrubbing too hard, because this can irritate the skin and trigger an attack.
Alternative Names
Plaque psoriasis
Source: http://www.nlm.nih.gov/medlineplus/ency/article/000434.htm

