Pleurisy and Other Pleural Disorders
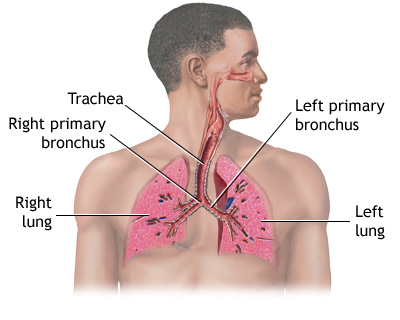
Pleurisy (PLUR-ih-se) is a condition in which the pleura is inflamed. The pleura is a membrane that consists of two large, thin layers of tissue. One layer wraps around the outside of your lungs. The other layer lines the inside of your chest cavity.
Between the layers of tissue is a very thin space called the pleural space. Normally this space is filled with a small amount of fluid—about 4 teaspoons full. The fluid helps the two layers of the pleura glide smoothly past each other as you breathe in and out.
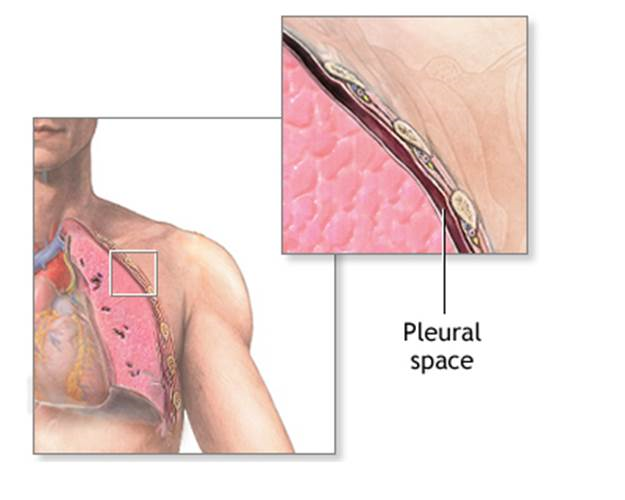
Pleurisy occurs if the two layers of the pleura become irritated and inflamed. Instead of gliding smoothly past each other, they rub together every time you breathe in. The rubbing can cause sharp pain.
Many conditions can cause pleurisy, including viral infections.
Other Pleural Disorders
Pneumothorax
Air or gas can build up in the pleural space. When this happens, it's called a pneumothorax (noo-mo-THOR-aks). A lung disease or acute lung injury can cause a pneumothorax.
Some lung procedures also can cause a pneumothorax. Examples include lung surgery, drainage of fluid with a needle, bronchoscopy (bron-KOS-ko-pee), and mechanical ventilation.
Sometimes the cause of a pneumothorax isn't known.
The most common symptoms of a pneumothorax are sudden pain in one side of the lung and shortness of breath. The air or gas in the pleural space also can put pressure on the lung and cause it to collapse.
Pleurisy and Pneumothorax
A small pneumothorax may go away without treatment. A large pneumothorax may require a procedure to remove air or gas from the pleural space.
A very large pneumothorax can interfere with blood flow through your chest and cause your blood pressure to drop. This is called a tension pneumothorax.
Pleural Effusion
In some cases of pleurisy, excess fluid builds up in the pleural space. This is called a pleural effusion. A lot of extra fluid can push the pleura against your lung until the lung, or part of it, collapses. This can make it hard for you to breathe.
Sometimes the extra fluid gets infected and turns into an abscess. When this happens, it's called an empyema (em-pi-E-ma).
You can develop a pleural effusion even if you don't have pleurisy. For example, pneumonia, (nu-MO-ne-ah), heart failure, cancer, or pulmonary embolism (PULL-mun-ary EM-bo-lizm) can lead to a pleural effusion.
Hemothorax
Blood also can build up in the pleural space. This condition is called a hemothorax (he-mo-THOR-aks). An injury to your chest, chest or heart surgery, or lung or pleural cancer can cause a hemothorax.
A hemothorax can put pressure on the lung and cause it to collapse. A hemothorax also can cause shock. In shock, not enough blood and oxygen reach your body's vital organs.
Outlook
Pleurisy and other pleural disorders can be serious, depending on their causes. If the condition that caused the pleurisy or other pleural disorder isn't too serious and is diagnosed and treated early, you usually can expect a full recovery.
Other Names for Pleurisy and Other Pleural Disorders
- Pleurisy also is called pleuritis and pleuritic chest pain.
- Pleural effusion also is called fluid in the chest and pleural fluid.
- Pneumothorax also is called air around the lung and air outside the lung
What Causes Pleurisy and Other Pleural Disorders?
Pleurisy
Many conditions can cause pleurisy. Viral infections are likely the most common cause. Other causes of pleurisy include:
- Bacterial infections, such as pneumonia (nu-MO-ne-ah) and tuberculosis, and infections from fungi or parasites
- Pulmonary embolism, a blood clot that travels through the blood vessels to the lungs
- Autoimmune disorders, such as lupus and rheumatoid arthritis
- Cancer, such as lung cancer, lymphoma, and mesothelioma (MEZ-o-thee-lee-O-ma)
- Chest and heart surgery, especially coronary artery bypass grafting
- Lung diseases, such as LAM (lymphangioleiomyomatosis) or asbestosis (as-bes-TO-sis)
- Inflammatory bowel disease
- Familial Mediterranean fever, an inherited condition that often causes fever and swelling in the abdomen or lungs
Other causes of pleurisy include chest injuries, pancreatitis (an inflamed pancreas), and reactions to certain medicines. Reactions to certain medicines can cause a condition similar to lupus. These medicines include procainamide, hydralazine, and isoniazid.
Sometimes doctors can't find the cause of pleurisy.
Pneumothorax
Lung diseases or acute lung injury can make it more likely that you will develop a pneumothorax (a buildup of air or gas in the pleural space). Such lung diseases may includeCOPD (chronic obstructive pulmonary disease), tuberculosis, and LAM.
Surgery or a chest injury also may cause a pneumothorax.
You can develop a pneumothorax without having a recognized lung disease or chest injury. This is called a spontaneous pneumothorax. Smoking increases your risk of spontaneous pneumothorax. Having a family history of the condition also increases your risk.
Pleural Effusion
The most common cause of a pleural effusion (a buildup of fluid in the pleural space) is heart failure. Lung cancer, LAM, pneumonia, tuberculosis, and other lung infections also can lead to a pleural effusion.
Sometimes kidney or liver disease can cause fluid to build up in the pleural space. Asbestosis, sarcoidosis (sar-koy-DO-sis), and reactions to some medicines also can lead to a pleural effusion.
Hemothorax
An injury to the chest, chest or heart surgery, or lung or pleural cancer can cause a hemothorax (buildup of blood in the pleural space).
A hemothorax also can be a complication of an infection (for example, pneumonia), tuberculosis, or a spontaneous pneumothorax.
What Are the Signs and Symptoms of Pleurisy and Other Pleural Disorders
Pleurisy
The main symptom of pleurisy is a sharp or stabbing pain in your chest that gets worse when you breathe in deeply or cough or sneeze.
The pain may stay in one place or it may spread to your shoulders or back. Sometimes the pain becomes a fairly constant dull ache.
Depending on what's causing the pleurisy, you may have other symptoms, such as:
- Shortness of breath or rapid, shallow breathing
- Coughing
- Fever and chills
- Unexplained weight loss
Pneumothorax
The symptoms of pneumothorax include:
- Sudden, sharp chest pain that gets worse when you breathe in deeply or cough
- Shortness of breath
- Chest tightness
- Easy fatigue (tiredness)
- A rapid heart rate
- A bluish tint to the skin caused by lack of oxygen
Other symptoms of pneumothorax include flaring of the nostrils; anxiety, stress, and tension; and hypotension (low blood pressure).
Pleural Effusion
Pleural effusion often has no symptoms.
Hemothorax
The symptoms of hemothorax often are similar to those of pneumothorax. They include:
- Chest pain
- Shortness of breath
- Respiratory failure
- A rapid heart rate
- Anxiety
- Restlessness
How Are Pleurisy and Other Pleural Disorders Diagnosed?
Your doctor will diagnose pleurisy or another pleural disorder based on your medical history, a physical exam, and test results.
Your doctor will want to rule out other causes of your symptoms. He or she also will want to find the underlying cause of the pleurisy or other pleural disorder so it can be treated.
Medical History
Your doctor may ask detailed questions about your medical history. He or she likely will ask you to describe any pain, especially:
- What it feels like
- Where it's located and whether you can feel it in your arms, jaw, or shoulders
- When it started and whether it goes away and then comes back
- What makes it better or worse
Your doctor also may ask whether you have other symptoms, such as shortness of breath,coughing, or palpitations. Palpitations are feelings that your heart is skipping a beat, fluttering, or beating too hard or fast.
Your doctor also may ask whether you've ever:
- Had heart disease.
- Smoked.
- Traveled to places where you may have been exposed to tuberculosis.
- Had a job that exposed you to asbestos. Asbestos is a mineral that, at one time, was widely used in many industries.
Your doctor also may ask about medicines you take or have taken. Reactions to some medicines can cause pleurisy or other pleural disorders.
Physical Exam
Your doctor will listen to your breathing with a stethoscope to find out whether your lungs are making any abnormal sounds.
If you have pleurisy, the inflamed layers of the pleura make a rough, scratchy sound as they rub against each other when you breathe. Doctors call this a pleural friction rub. If your doctor hears the friction rub, he or she will know that you have pleurisy.
If you have a pleural effusion, fluid buildup in the pleural space will prevent a friction rub. But if you have a lot of fluid, your doctor may hear a dull sound when he or she taps on your chest. Or, he or she may have trouble hearing any breathing sounds.
Muffled or dull breathing sounds also can be a sign of a pneumothorax (a buildup of air or gas in the pleural space).
Diagnostic Tests
Depending on the results of your physical exam, your doctor may recommend tests.
Chest X Ray
A chest x ray is a painless test that creates a picture of the structures in your chest, such as your heart, lungs, and blood vessels. This test may show air or fluid in the pleural space.
A chest x ray also may show what's causing a pleural disorder—for example, pneumonia, a fractured rib, or a lung tumor.
Sometimes a chest x ray is taken while you lie on your side. This position can show fluid that didn't appear on an x ray taken while you were standing.
Chest CT Scan
A chest computed tomography (to-MOG-rah-fee) scan, or chest CT scan, is a painless test that creates precise pictures of the structures in your chest.
This test provides a computer-generated picture of your lungs that can show pockets of fluid. A chest CT scan also may show signs of pneumonia, a lung abscess, a tumor, or other possible causes of pleural disorders.
Ultrasound
This test uses sound waves to create pictures of your lungs. An ultrasound may show where fluid is located in your chest. The test also can show some tumors.
Chest MRI
A chest magnetic resonance imaging scan, or chest MRI, uses radio waves, magnets, and a computer to created detailed pictures of the structures in your chest. This test can show pleural effusions and tumors.
This test also is called a magnetic resonance (MR) scan or a nuclear magnetic resonance (NMR) scan.
Blood Tests
Blood tests can show whether you have an illness that increases your risk of pleurisy or another pleural disorder. Such illnesses include bacterial or viral infections, pneumonia, pancreatitis (an inflamed pancreas), kidney disease, or lupus.
Arterial Blood Gas Test
For this test, a blood sample is taken from an artery, usually in your wrist. The blood's oxygen and carbon dioxide levels are checked. This test shows how well your lungs are taking in oxygen.
Thoracentesis
Once your doctor knows whether fluid has built up in the pleural space and where it is, he or she can remove a sample for testing. This is done using a procedure called thoracentesis (THOR-ah-sen-TE-sis).
During the procedure, your doctor inserts a thin needle or plastic tube into the pleural space and draws out the excess fluid. After the fluid is removed from your chest, it's sent for testing.
The risks of thoracentesis—such as pain, bleeding, and infection—usually are minor. They get better on their own, or they're easily treated. Your doctor may do a chest x ray after the procedure to check for complications.
Fluid Analysis
The fluid removed during thoracentesis is examined under a microscope. It's checked for signs of infection, cancer, or other conditions that can cause fluid or blood to build up in the pleural space.
Biopsy
Your doctor may suspect that tuberculosis or cancer has caused fluid to build up in your pleural space. If so, he or she may want to look at a small piece of the pleura under a microscope.
To take a tissue sample, your doctor may do one of the following procedures:
- Insert a needle into your chest to remove a small sample of the pleura's outer layer.
- Insert a tube with a light on the end (endoscope) into tiny cuts in your chest wall so that he or she can see the pleura. Your doctor can then snip out small pieces of tissue. This procedure must be done in a hospital. You'll be given medicine to make you sleep during the procedure.
- Snip out a sample of the pleura through a small cut in your chest wall. This is called an open pleural biopsy. It's usually done if the sample from the needle biopsy is too small for an accurate diagnosis. This procedure must be done in a hospital. You'll be given medicine to make you sleep during the procedure.
How Are Pleurisy and Other Pleural Disorders Treated?
Pleurisy and other pleural disorders are treated with procedures, medicines, and other methods. The goals of treatment include:
- Relieving symptoms
- Removing the fluid, air, or blood from the pleural space (if a large amount is present)
- Treating the underlying condition
Relieving Symptoms
To relieve pleurisy symptoms, your doctor may recommend:
- Acetaminophen or anti-inflammatory medicines (such as ibuprofen) to control pain.
- Codeine-based cough syrups to control coughing.
- Lying on your painful side. This might make you more comfortable.
- Breathing deeply and coughing to clear mucus as the pain eases. Otherwise, you may develop pneumonia.
- Getting plenty of rest.
Removing Fluid, Air, or Blood From the Pleural Space
Your doctor may recommend removing fluid, air, or blood from your pleural space to prevent a lung collapse.
The procedures used to drain fluid, air, or blood from the pleural space are similar.
- During thoracentesis, your doctor will insert a thin needle or plastic tube into the pleural space. An attached syringe will draw fluid out of your chest. This procedure can remove more than 6 cups of fluid at a time.
- If your doctor needs to remove a lot of fluid, he or she may use a chest tube. Your doctor will inject a painkiller into the area of your chest wall where the fluid is. He or she will then insert a plastic tube into your chest between two ribs. The tube will be connected to a box that suctions out the fluid. Your doctor will use a chest x ray to check the tube's position.
- Your doctor also can use a chest tube to drain blood and air from the pleural space. This process can take several days. The tube will be left in place, and you'll likely stay in the hospital during this time.
Sometimes the fluid in the pleural space contains thick pus or blood clots. It may form a hard skin or peel, which makes the fluid harder to drain. To help break up the pus or blood clots, your doctor may use a chest tube to deliver medicines called fibrinolytics to the pleural space. If the fluid still won't drain, you may need surgery.
If you have a small, persistent air leak into the pleural space, your doctor may attach a one-way valve to the chest tube. The valve allows air to exit the pleural space, but not reenter. Using this type of valve may allow you to continue your treatment from home.
Treat the Underlying Condition
The fluid sample that was removed during thoracentesis will be checked under a microscope. This can tell your doctor what's causing the fluid buildup, and he or she can decide the best way to treat it.
If the fluid is infected, treatment will involve antibiotics and drainage. If you have tuberculosis or a fungal infection, treatment will involve long-term use of antibiotics or antifungal medicines.
If tumors in the pleura are causing fluid buildup, the fluid may quickly build up again after it's drained. Sometimes antitumor medicines will prevent further fluid buildup. If they don't, your doctor may seal the pleural space. Sealing the pleural space is called pleurodesis (plur-OD-eh-sis).
For this procedure, your doctor will drain all of the fluid out of your chest through a chest tube. Then he or she will push a substance through the chest tube into the pleural space. The substance will irritate the surface of the pleura. This will cause the two layers of the pleura to stick together, preventing more fluid from building up.
Chemotherapy or radiation treatment also may be used to reduce the size of the tumors.
If heart failure is causing fluid buildup, treatment usually includes diuretics (medicines that help reduce fluid buildup) and other medicines.
Source: http://www.nhlbi.nih.gov/health/health-topics/topics/pleurisy/

